Carbohydrate Source in Higher Protein Diets
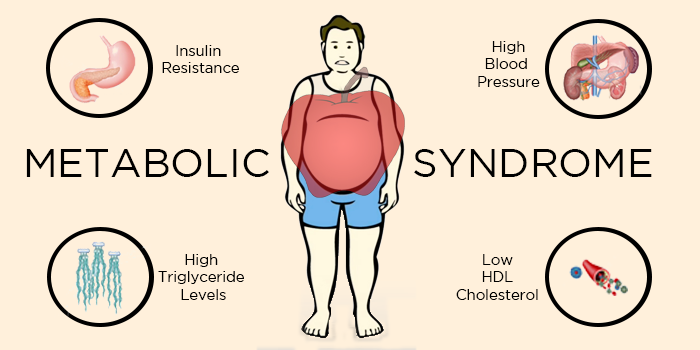
Metabolic syndrome (MetS) within the United States is rapidly increasing, with approximately one in three adults qualifying for a diagnosis.1,2 MetS is defined as a grouping of cardiometabolic risk factors including insulin resistance, visceral adiposity, atherogenic dyslipidemia, and endothelial dysfunction3. Each risk factor has its detrimental effects; however, when these risk factors are clustered together, they can have an even greater impact on cardiovascular health.4 If left untreated, the cardiometabolic risk factors of MetS contribute to the development of cardiovascular disease and type 2 diabetes.5
Currently, there are two primary approaches used to treat and manage MetS: pharmacological and/or lifestyle (e.g. physical activity, nutrition/dietary intake) modification.6 Recently, higher protein diets (HPD) (approximately 28–30% of macronutrient content) and their effects on cardiovascular health have been the subject of much investigation.6-16
Ada-Miette Thomas and fellow researchers at the University of Arkansas Center for Human Nutrition aimed to determine the role of the carbohydrate source with an HPD on cardiometabolic biomarkers in adults at risk for MetS. Two dietary interventions were conducted: 1) to determine the short-term effects of a carbohydrate source with an HPD on biomarkers in adults at risk for MetS and 2) to determine the long-term effect of a carbohydrate source with an HPD on cardiometabolic biomarkers in adults at risk for MetS.17
In dietary intervention 1, a 240-minute acute randomized, controlled study (n = 23; 15 females and 8 males; age = 35.7 ± 6.0 y, weight 100.65 ± 5.44 kg, body mass index (BMI) 36.4 ± 2.5 kg/m2), participants consumed a higher protein test breakfast containing white potatoes or a control carbohydrate (white rice) and were evaluated for the response of appetite, palatability, and fasting glucose and insulin. At each of 0, 30, 60, 120, 180, and 240 minutes, a 10 ml whole blood sample was collected, and a visual analog scale (VAS) on subjective appetite was completed. At minute 15, a VAS on the subjective palatability of the test breakfast was collected. There were no significant differences in markers of appetite, palatability, or cardiometabolic response between treatment groups. Consumption of a higher protein test breakfast containing white potatoes did not show an overall improvement in markers of appetite, palatability, and cardiometabolic response compared to a higher protein test breakfast containing white rice in adults at risk for MetS.
In dietary intervention 2, participants (n = 21; 14 females and 7 males, age = 35.36 ± 6.17 y, BMI = 35.82 ± 3.29 kg/m2) were recruited to participate in a 16-week randomized, controlled dietary intervention. To qualify, participants needed two of the five criteria of MetS outlined by NCEP ATP III (2005). Upon recruitment, participants were assigned to one of two dietary intervention groups: 1) higher protein intake (30%) and 4-6 meals per week containing white potatoes (HPWP); or 2) higher protein intake (30% of energy) with 4-6 meals per week containing starchy carbohydrates (white rice/pasta) and no potato consumption (HPCC). Participants were advised to maintain their normal calorie intake and physical activity levels throughout the study. Participants arrived fasted and anthropometrics and biomarkers of MetS were measured at 0, 4, 8, and 16 weeks.
Two-way analysis of variance (ANOVA) was used to determine the effect of diet, time, and diet over time (p-value ≤ 0.05). HPWP had significant changes in weight, total cholesterol, LDL-cholesterol, lean mass, fat-free mass, and bone mineral content when compared to HPCC. However, no significant differences were seen between dietary treatment groups in measurements of fasting plasma glucose, insulin, or cortisol. Consumption of an HPD containing white potatoes improved markers of body composition and cholesterol but did not significantly affect cardiometabolic biomarkers of MetS when compared to an HPD containing a control carbohydrate like white rice.
Collectively, the results of this study suggest that consumption of an HPD containing white potatoes will not affect markers of MetS. However, there is potential for carbohydrate sources to be useful in the treatment of markers of MetS. Additional research is necessary to validate these findings.
References
- Monteiro, R. Azevedo, I. 2010. Chronic inflammation in obesity and the metabolic syndrome. Mediators of Inflam. 2010:1-10.
- Saklayen, M.G. 2018. The global epidemic of the metabolic syndrome. Current Hypertension Rep. 20(2).
- Huang, P.L. 2009. A comprehensive definition for metabolic syndrome. Disease Models Mechan.2(5-6):231-237.
- Papakonstantinou, E., et al. 2013. Metabolic syndrome and cardiometabolic risk factors. Curr. Vasc. Pharmacol.11(6):858-79.
- Cooke, A.A., et al. 2016. Fatty acids and chronic low grade inflammation associated with obesity and the metabolic syndrome. Eur. J. Pharmacol. 785:207-214.
- Wagh, A., Stone, N.J. 2004. Treatment of metabolic syndrome. Expert Rev. Cardiovasc. Ther. 2(2):213-228.
- Hu, F.B. 2005. Protein, body weight, and cardiovascular health. Am. J. Clin. Nutr. 82(1):242S-247S.
- Yılmaz, S.K., et al. 2021. Effect of different protein diets on weight loss, inflammatory markers, and cardiometabolic risk factors in obese women. J. Res. Med. Sci. 26: 28.
- Mitra, S.R., Tan, P.Y. 2019. Effect of an individualised high-protein, energy-restricted diet on anthropometric and cardio-metabolic parameters in overweight and obese Malaysian adults: a 6-month randomised controlled study. Br. J. Nutr. 121(9):1002-1017.
- Huang, G., et al. 2021. Effect of protein intake on visceral abdominal fat and metabolic biomarkers in older men with functional limitations: Results from a randomized clinical trial. J. Gerontol. Biol. Sci. Med. Sci. 76(6):1084-1089.
- Dorenbos, E., et al. 2021. Effect of a high protein/low glycaemic index diet on insulin resistance in adolescents with overweight/obesity—A randomized clinical trial. Pediatric Obesity. 16(1).
- Evangelista, L.S., et al. 2021. High‐protein vs. standard‐protein diets in overweight and obese patients with heart failure and diabetes mellitus: findings of the Pro‐HEART trial. ESC Heart Failure. 8(2):1342-1348.
- Wycherley, T.P., et al. 2012. Comparison of the effects of 52 weeks weight loss with either a high-protein or high-carbohydrate diet on body composition and cardiometabolic risk factors in overweight and obese males. Nutr. Diabetes. 2(8):e40-e40.
- Johnstone, A.M., et al. 2011. Effects of a high-protein, low-carbohydrate high-protein, moderate-carbohydrate weight-loss diet on antioxidant status, endothelial markers and plasma indices of the cardiometabolic profile. Br. J. Nutr.106(2):282-291.
- Mok, A., et al. 2015. Postprandial changes in cardiometabolic disease risk in young Chinese men following isocaloric high or low protein diets, stratified by either high or low meal frequency - A randomized controlled crossover trial. Nutr. J. 15(1).
- Lobley, G.E., et al. 2015. Responses in gut hormones and hunger to diets with either high protein or a mixture of protein plus free amino acids supplied under weight-loss conditions. Br. J. Nutr. 113(8):1254-1270.
- Thomas, A.M., et al. 2023. Effect of carbohydrate source in a higher protein diet on body weight, body composition, and metabolic health outcomes in adults at risk for type 2 diabetes. Am. Physiol. Society. doi:10.1152/physiol.2023.38.S1.5735114.
Follow us on LinkedIn for the latest updates on all things happening here at BSM Partners.
About the Author
Ada-Miette Thomas is a senior analyst at BSM Partners. She received both bachelor’s and master’s degrees in food science with an emphasis on nutrition. Ada-Miette conducted research with a focus on human nutrition and studied the effects of carbohydrate sources on markers of Metabolic Syndrome in adults.
This content is the property of BSM Partners. Reproduction or retransmission or repurposing of any portion of this content is expressly prohibited without the approval of BSM Partners and is governed by the terms and conditions explained here.